Testing for Dry Eye Syndrome in NYC
Over the last several years there have been numerous laboratory tests that have become available to provide the dry eye specialist information to help assess the patient’ dry eyes. This information can be used to differentiate different types of dry eyes and to assist in developing the best dry eye treatment regimen. As part of your dry eye evaluation at Pamel Vision and Laser Group, you will be advised to undergo a series of laboratory tests as part of a treatment plan.
Click the testing categories below to learn more about dry eye assessments
Lab Tests
At-Home Tests
In-Office Testing
Laboratory Testing for Dry Eyes
Tear Osmolarity Test

Tear Osmolarity Test
The TearLab test is a quick test that measures how concentrated the electrolytes in your tears are. Higher levels signify that the aqueous component of the tears is low. To administer the test, the physician or technician takes a small sample of a patient’s tears from each eye using a special pen and sample card.
The TearLab device analyzes the card and provides a read out of the osmolarity level in the sample. A reading of greater than 307 mOsms/L is considered a sign of dry eyes. The severity of dryness increases with increasing osmolarity levels. A difference between the eyes, where one is high and the other normal, is a red flag as well. This test can easily be repeated after therapy has been initiated to show improvement in dry eyes. The test does not differentiate between aqueous deficient and evaporative dry eye.
MMP-9 Test
MMP-9 is an inflammatory marker (a cytokine produced by epithelial cells) that is consistently elevated in the tears of patients with dry eye and ocular surface disease. The test is easily performed in the office and is inexpensive. It involves a small applicator that is touched to the surface of the eye. Without adequate lubrication from the tear layer, the eyelids can cause friction and shearing forces to the ocular surface creating pain and discomfort and increasing the levels of MMP-9.
Lactoferrin Test
Lactoferrin is a protein produced by the acinar cells of the lacrimal gland and is present in the normal tear film. It has antimicrobial properties and is reduced in patients with aqueous tear deficiency. This test is used in patients with symptoms such as foreign body sensation, burning, or intermittent blurring of vision. It is also use in patients who are contact lens intolerant. It is useful in diagnosing Sjögrens Syndrome dry eye and non Sjögrens Syndrome dry eye. The test involves assaying the person’s tear film by taking a very small sample. The doctors at Pamel Vision and Laser Group will determine if you should have this level measured as part of your dry eye assessment. In addition the test can be repeated to monitor improvement in the patients’ dry eyes after treatment has been initiated.
Immunoglobulin E Levels:
Immunoglobulin E (IgE) is an antibody only found in mammals. Tear IgE (IgE located in the natural tears of the eye) has long been established as the key immunologic mechanism in allergic conjunctivitis and the measurement of tear IgE concentrations can be used to confirm the condition. Because total IgE in tear fluid increases with the severity of the allergic response, determining the total IgE concentration is useful for making a clinical diagnosis of allergic conjunctivitis and also for determining the severity of the allergic presentation.
In dry eye disease, the presence of an allergen often mimics the signs and symptoms of dry eye disease, so it is clinically useful to assess the presence of an allergen during the initial dry eye workup to confirm, or rule out, its presence. The evaluation of IgE levels and tear dynamics are important for the differential diagnosis of patients with allergic conjunctivitis and dry eye.
Sjögren’s Syndrome Lab Test: Sjö Test
Sjögren’s Syndrome is one of the most common rheumatologic conditions and the second most common systemic cause of dry eye. It is underdiagnosed because the testing is highly unreliable. Recently, a simple in-office blood test for Sjögren’s Syndrome called Sjö has been approved and tests for biomarkers that detect Sjögrens Syndrome earlier and with higher sensitivity and specificity. The test is a quick finger-prick test and the results will be sent to the lab to be evaluated. Once your test results become available, your dry eye specialist will contact you to discuss them. Results are received typically within a week.
At-Home Diagnostic Tests for Dry Eyes
There are numerous diagnostic tests performed in the office that assist physicians at Pamel Vision and Laser Group in diagnosing and treating ocular surface disease and dry eye. Please find copies of our questionnaires located in the link below. You may complete this at home and if you find your score to be over 10 please call to set an appointment for evaluation.
Ocular Surface Disease Index
SPEED Questionnaire
Ocular Surface Assessment at Pamel Vision and Laser Group
The ocular surface assessment is performed by our doctors at Pamel Vision and Laser Group. Evaluation of the ocular surface under the biomicroscope looks at the extent of damage and causes of disease. Frequently various diagnostic dyes are introduced to the eye to differentiate causes of cellular damage.
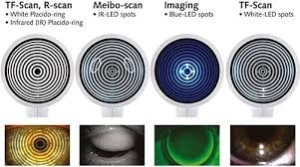
Tear Break Up Time (TBUT)
Blephex device for blepharitis treatment
TBUT is an advanced measurement of the break up time of the tear film on the eyes. This measures the quality of the protective lipid layer and the effect of evaporation on the eyes. A low TBUT is associated with lipid layer deficiency leaving the eye prone to evaporative conditions. The advanced measurement tools at the Dry Eye and Ocular Surface Disease Center at Pamel Vision and Laser Group ensure for accurate and reproducible results for comparison and tracking of progress.
Schirmer’s Testing
Schirmer’s testing is a measurement of aqueous tear production that is produced by the lacrimal and accessory lacrimal glands. It is performed in the office using specialized strips of cellulose paper that can measure the amount of aqueous tear production. This test does not have the diagnostic power to determine the cause of dry eye and can be positive in a number of situations.
Lissamine Green Stain

Lissamine green stain of the ocular surface in a dry eye patient
Lissamine green has broad applicability as a dye, and is widely used as a non-ophthalmic drug, cosmetic and food additive. As a diagnostic tool in ophthalmology, lissamine green preferentially stains membrane-damaged or devitalized cells on the surface of the eye. Lissamine is unique in that it does not stain healthy ocular surface cells. It is an effective visual way for physicians to assess the ocular surface in patients with ocular surface disease and dry eyes. This stain used in every patient who undergoes a dry eye evaluation at Pamel Vision and Laser Group.
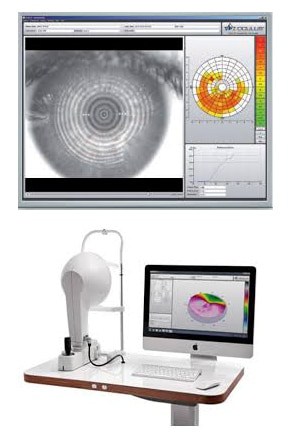
Interferometry
Interferometry is the evaluation of precorneal tear film. In dry eye interferometry helps to understand the tear film dynamics and assess the lipid and aqueous layers of the tear film.
Tear Meniscus Measurement
The tear meniscus is the reservoir of tears that rests on the lower eyelid margin. After each blink this meniscus is spread across the ocular surface to provide clear vision, lubricative comfort, and anti-microbial properties. In dry eye and ocular surface disease this prism can be deficient. By using specialized instrumentation using repeatable and accurate measurements we are able to measure the depth of the prism at the beginning and throughout the treatment process to insure progress is being made.
Lipid Secretion Assessment
 The lipid layer of the tear film is created by specific type of glands- the meibomian glands-located in the eyelids. At Pamel Vision and Laser Group, the doctors utilize a gentle expression technique to assess the production, quantity, and quality of the oils from these glands.
The lipid layer of the tear film is created by specific type of glands- the meibomian glands-located in the eyelids. At Pamel Vision and Laser Group, the doctors utilize a gentle expression technique to assess the production, quantity, and quality of the oils from these glands.
Ocular Surface Photography
Documentation of the ocular surface is paramount to track progress during treatment. We collect baseline images to aid in assessment by using advanced and specialized photography equipment.
Meibography
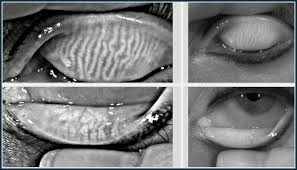
Meibography to assess the
lipid-producing meibomian glands
This test allows for assessment of the oil glands (meibomian glands) by using IR spectral photography to image the entire gland. The images allow us to measure the amount of active glands, the size, and the shape. In some cases individuals with severe dry eye have a condition known as meibomian gland dropout in which the meibomian glands have atrophied leaving the eye with a severe lipid layer deficiency that results in extreme evaporative dry eye.





