Keratoconus Treatment in NYC
Dr. Gregory Pamel is a premier eye surgeon in Manhattan who offers a wide range of vision correction procedures and complex treatments for corneal diseases to his New York City patients. In the sections below, Dr. Pamel, a renowned Manhattan / New York City keratoconus and ectasia treatment provider, discusses keratoconus and ectasia as well as the latest and most effective treatment options.
What is cornea and its function?
The cornea is the transparent tissue that covers the anterior surface of the eye and is responsible for focusing incoming light rays onto the retina. A normal cornea can focus incoming light rays onto the retina either naturally (by the cornea itself) or with corrective eyewear. The cornea is made up primarily of collagen and water and is prone to a number of diseases that can interfere with its ability to focus light rays onto the retina.
What is Astigmatism?
Astigmatism is a common corneal condition. In “regular” astigmatism, the cornea is shaped like a football instead of a basketball. Individuals with “regular” astigmatism require glasses or contact lenses.
What is Keratoconus?
Keratoconus is a disorder that leads to thinning of the cornea, inducing a “cone-like” shape and creating an irregular surface. In patients with keratoconus, the light rays focused onto the retina are distorted. This leads to blurred vision and “irregular” astigmatism, which cannot be corrected with glasses or contact lenses.
This disorder has an incidence of approximately 1 in 2,000 individuals in the general population. It usually affects both eyes, with one eye being more affected than the other. Keratoconus affects males and females in equal frequency, and there is no ethnic or racial predilection. It usually first appears in puberty and progresses until the early 30s, although the rate of progression is impossible to predict. Some patients have a mild form of the condition (forme fruste), which may go undetected for years.
Post-LASIK Ectasia
In 1998, it was noted that certain patients who had undergone the LASIK procedure had developed a keratoconus-like disorder called “post-LASIK ectasia.” Post-LASIK Ectasia is often described as keratoconus in someone who has previously undergone the LASIK procedure. The incidence of post-LASIK ectasia is thought to be approximately 1 in 1,000 patients. It is thought that the LASIK procedure – since it involves the removal of corneal tissue with the laser – results in a permanent weakening of the cornea, which then leads to post-LASIK ectasia.
Post-LASIK Ectasia can occur not only after LASIK but also after PRK (photorefractive keratectomy). Patients who have post-LASIK ectasia experience a decrease in best corrected visual acuity several months or years after they have undergone their LASIK or PRK procedure. Post-LASIK Ectasia is diagnosed with corneal topography and the Pentacam device, which shows a steepening of the cornea, similar to what is seen in keratoconus.
Risk Factors
Several risk factors for post-LASIK ectasia have been reported in the ophthalmic literature, such as thin corneas, high myopia, high preoperative keratometry values, preoperative irregular astigmatism and young age. A risk factor scoring system has been developed and published in a peer reviewed medical journal (Randelman, B.J. et al. Ophthalmology 2008 Vol. 115) to assign a score for developing post-LASIK ectasia after LASIK. Factors include preoperative corneal topography pattern, residual corneal stromal bed thickness, age, preoperative corneal thickness and preoperative spherical equivalent (which is the prescription measured by the doctor prior to the LASIK procedure). This scoring system identified 92 percent of patients who were at risk for developing post-LASIK ectasia. Dr. Pamel uses this scoring system to determine your candidacy for LASIK eye surgery.
However, other studies have found that a large number of patients who had the same risk factors did not develop post-LASIK ectasia (Binder, P.S. Journal of Cataract and Refractive Surgery 2007 33(9) 1530-1538). Why certain patients develop post-LASIK ectasia after LASIK is not fully understood. It most likely involves biomechanical factors related to the cornea.
What Causes Keratoconus?
While genetic factors play a role in keratoconus, only 13-15 percent of patients with keratoconus have a family history of the disease. Gene therapy, which is not yet available, may ultimately be the only treatment that can potentially cure this disease. There are a number of genetic conditions associated with keratoconus, which include a history of allergies and atopy, Down syndrome, Ehlers-Danlos syndrome and Leber’s congenital amaurosis.
Several theories have attempted to explain the cause of keratoconus, but none have been proven. Eye rubbing is one such theory. Patients with keratoconus often report that they frequently rub their eyes. Since patients with keratoconus have a greater incidence of allergies and atopy, eye rubbing may be a response to the allergy, which in turn may lead to the development of keratoconus. Keratoconus patients are strongly advised not to rub their eyes, since this may influence the progression of the disease. In patients who have undergone LASIK, eye rubbing may be a cause of post-LASIK ectasia, so patients should be instructed to avoid vigorous eye rubbing after LASIK. Allergic symptoms of the eyes such as itching, redness and tearing should be treated with topical anti-allergy medication.
 A deficiency in collagen crosslinking is another potential cause of keratoconus. Crosslinking of collagen is necessary for the biomechanical stability of the cornea, and free radicals are thought to interfere with crosslinking in keratoconus patients. Corneal crosslinking using riboflavin and ultraviolet light has been used to halt and reverse the progression of keratoconus in a number of studies. Dr. Pamel was one of the first eye surgeons in New York to become involved in crosslinking as a treatment for keratoconus as part of an FDA clinical trial.
A deficiency in collagen crosslinking is another potential cause of keratoconus. Crosslinking of collagen is necessary for the biomechanical stability of the cornea, and free radicals are thought to interfere with crosslinking in keratoconus patients. Corneal crosslinking using riboflavin and ultraviolet light has been used to halt and reverse the progression of keratoconus in a number of studies. Dr. Pamel was one of the first eye surgeons in New York to become involved in crosslinking as a treatment for keratoconus as part of an FDA clinical trial.
Diagnosis of Keratoconus
Patients who suffer from keratoconus often visit an eye care specialist unaware of any problem other than blurry vision. Often, the patients’ eyeglass prescription will change but without any improvement in visual acuity. Rigid gas permeable contact lenses are needed to fully correct vision in patients with keratoconus. During a routine eye exam, the physician may detect subtle signs of keratoconus at the slit lamp, but the best way to diagnose the condition is with a topographical map of the cornea (corneal topography), which reveals an irregular shape in patients who have the condition.
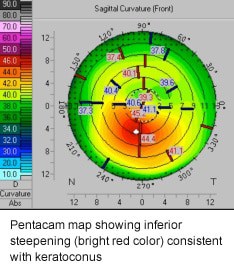 In addition, a device known as the Pentacam uses a camera to take 50 cross sectional views of the cornea. The Pentacam maps show irregularity both on the front surface and the back surface of the cornea. They also provide a thickness map of the cornea, which shows areas of thinning in eyes affected by keratoconus.
In addition, a device known as the Pentacam uses a camera to take 50 cross sectional views of the cornea. The Pentacam maps show irregularity both on the front surface and the back surface of the cornea. They also provide a thickness map of the cornea, which shows areas of thinning in eyes affected by keratoconus.
Keratoconus Treatment Options
Corneal Collagen Crosslinking
CXL, an advanced keratoconus and post-LASIK ectasia treatment, involves ultraviolet light in combination with topically applied riboflavin (vitamin B) eye drops to increase the crosslinking of the collagen fibers, which in turn strengthens the cornea.
Read more about corneal crosslinking.
Contact Lenses
In the early stages of keratoconus, patients are often able to see clearly with spectacles or soft contact lenses. As the condition worsens, and the shape of the cornea becomes more irregular, rigid gas permeable (RGP) lenses are often necessary to provide clear vision. RGP lenses eliminate the irregularity of the cornea and allow the incoming light rays to focus clearly onto the retina.
Another type of contact lens for keratoconus is the piggyback lens, in which a soft contact lens is fit first on the eye and an RGP lens piggybacks on top of the soft lens. This is often used when the patient cannot tolerate an RGP lens by itself. Hybrid lenses, which consist of an RGP center and a soft skirt, can also be used.
Dr. Pamel works with a number of contact lens physicians who specialize in fitting patients with keratoconus.
Corneal Transplant/Deep Anterior Lamellar Keratoplasty Procedures
The corneal transplant surgery is performed on patients with advanced keratoconus who cannot wear contact lenses or who would not improve with the corneal crosslinking procedure.
A new procedure called DALK (deep anterior lamellar keratectomy) is increasingly being performed on patients with keratoconus or ectasia. The treatment spares the endothelial layer of the patient’s cornea. The endothelial layer is the back layer of the cornea that is usually not affected by keratoconus or ectasia. In the DALK procedure, the cornea anterior to the endothelium is replaced with a donor cornea. The patient’s own endothelium is preserved.
Studies have shown that a patient’s own endothelium remains healthier than a transplanted endothelium. In addition, preserving a patient’s endothelium will decrease the chances of endothelial rejection, which can occur during a full thickness corneal transplant. Dr. Pamel was one of the first surgeons in New York to perform the DALK procedure and believes it offers the patient the best chance for long-term survival of the corneal transplant.
Keratoconus FAQs
What are the symptoms of keratoconus?
 Keratoconus develops slowly, generally beginning in a patient’s teenage years or early 20s. Patients often notice their vision get progressively worse or blurry. They can also experience light sensitivity and notice halos around lights. Headaches are common. At a certain point, they may also recognize their thinning cornea jut outward into a conical shape.
Keratoconus develops slowly, generally beginning in a patient’s teenage years or early 20s. Patients often notice their vision get progressively worse or blurry. They can also experience light sensitivity and notice halos around lights. Headaches are common. At a certain point, they may also recognize their thinning cornea jut outward into a conical shape.
Why is early detection important?
Keratoconus treatments like corneal crosslinking have been found extremely effective at slowing or even stopping the progression of keratoconus. The earlier a doctor can diagnose and treat keratoconus, the more vision can be preserved. Untreated keratoconus can steal so much of a person’s sight that it requires a corneal transplant, so it makes sense to undergo non-invasive treatment instead.
Which keratoconus treatment is the best choice for me?
Dr. Pamel has experience treating patients at beginning, intermediate and advanced stages of keratoconus. After assessing your eyes and how far keratoconus has progressed, Dr. Pamel can develop a treatment plan that is best for you. Corneal crosslinking is a great solution for many patients since it is an easy way to strengthen the cornea without the need for surgery. RGP contact lenses are also a reliable way to correct vision that has become imperfect due to keratoconus.
Contact Us
To learn more about keratoconus, schedule a consultation with Dr. Pamel at one of our New York City offices by calling (212) 355-2215.





